Micro-organisms are tiny living creatures, such as bacteria and viruses that are present in all environments. Although there are thousands of species, few invade the human body, multiply, and cause disease (Allan R., Tunkel B. ;2016); many live on the skin, in the mouth, upper airways, gut, and genitals (especially the vagina), without causing disease (commensal flora). Whether a microorganism lives as a harmless companion to humans or invades and causes disease depends on its nature and the condition of the person’s natural defenses. Infectious diseases are the most prevalent diseases, more than a third of hospitalized patients receive at least one antibiotic. A distinction is made between bacterial diseases caused by bacteria and viral diseases caused by viruses; bacteria and viruses are also called microbes, germs or micro-organisms. Infections can also be of fungal or parasitic origin (M. Neuman; 1979).
I. VIRUS
They are micro-organisms made of DNA or RNA covered by an envelope. They do not have the ability to multiply themselves. For this process, they must get inside cells of a living organism. They multiply inside these cells. When there are numerous of them present inside the cell, the cell is destroyed, releasing a large amount of virus that infects other cells (Okusa, 2012).
II. FUNGI
Fungi are microorganisms of plant origin that multiply autonomously and cause severe pathologies mostly in immuno-compromised patients (Okusa, 2012).
III. PARASITS
They are formed of several cells. During their existence they undergo a certain number of transformations. These transformations can take place in the external environment, in humans or in animals. All these transformations are required for the reproduction of the parasite (Merck Manual 2017).
The contaminations can be made by different mechanisms: Direct contamination mode, which requires a contact between the infected person and the healthy person and indirect contamination mode, where there is an intermediary between the infected person and the healthy person. The intermediary can be another person, water, an insect or even a reservoir (Okusa, 2012).
IV. BACTERIA
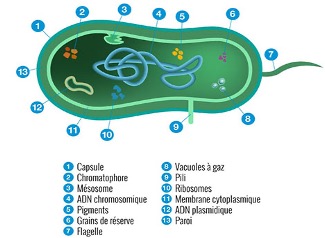
Bacteria are prokaryotic cells with a characteristic cel organization; they are ubiquitous and most of them have a direct or indirect beneficial effect for either their potential commercial use or for their action on the human organism (commensal flora) or on the surrounding environment in which we live (Mims et al., 1993). Compared to the large number of living bacteria, there are relatively few that cause pathologies with a significant impact on the well-being of humans. Their importance is such that the major ones have been well studied and are currently well known. However, new pathogens continue to emerge leading to the introduction of previously unknown infections, such as Photorhabdus asymbiotica, an entomopathogenic bacterium, which has recently been reported in the USA and Australia (Costa et al., 2010). The bacterial cells are small in size (0.3 to 0.5 μm). They can have two basic forms see (Fig. 2): the shell and the bacillus. Broadly speaking, a bacterium consists of (Mims et al., 1993; Kayser et al., 2008): The nucleoid (equivalent to the nucleus in eukaryotes), a circular, very thin, long DNA filament that is not surrounded by a membrane; there are also plasmids, which are nonessential genetic structures; The cytoplasm, which contains a large number of soluble compounds of varying molecular weights, RNA, and about 20,000 ribosomes per cell. Bacterial ribosomes are made up of proteins and ribosomal RNA, they are formed from the 30S and 50S subunits into 70S ribosomes and are the organelles of protein synthesis. The cytoplasm also contains substances of reserve like glycogen or lipids; The cytoplasmic membrane that is a typical elementary biological membrane, constituted by a double phospholipidic layer, in which are attached numerous proteins like permeases, enzymes notably for the synthesis of the cell wall, sensory proteins and, in aerobic bacteria, proteins of the respiratory chain; The cell wall, operating as an armor around the membrane, is constituted essentially by the murein. In Gram-negative bacteria, the cell wall has an additional outer layer, called the “outer membrane”, which is studded with pores and into which a significant lipopolysaccharide for the pathogenesis of Gram-negative infections is inserted. This outer membrane is absent in Gram-positive bacteria where the murein is thicker and contains a teichoic acid and wall-associated proteins that play a role in the pathogenesis of Gram-positive infections. The capsule is a structure found in many bacteria, it is made of polysaccharides and its role is to protect the bacteria from phagocytosis. Flagella are proteins that allow the bacteria to move actively by turning like a helix around an axis; fimbriae and pili are structures found outside the cell wall; their role is to allow the adhesion of bacteria to host cells. They can also play a role in the transfer of genetic elements from one bacterium to another (sexual pili). The biofilm is a structured set of bacterial cells, enveloped in a self-produced polymer matrix, which docks on inert surfaces or on living tissues. The biofilm can reach a significant thickness (a few millimeters) and the bacteria located in its depth are largely protected against immune cells, antibodies and antibiotics. The secreted polymers are often carbohydrate monosaccharides in networks called glycocalyx (“glycoside shell”).
Bacterial spores are persistent forms of a “vegetative” cell; they vary in shape from spherical to oval, they have a thick wall and are highly resistant to chemical or physical agents. Among the human pathogenic bacteria, only the genus Clostridium and Bacillus can form spores. The importance of spores in medicine lies mainly in their resistance to heat, thus requiring very high temperatures during sterilization.
Human pathogenic bacteria derive their energy from the degradation of organic nutrient compounds for new synthesis and secondary activities. Oxidation of energetic substrates results from the respiratory pathway (the electron and proton acceptor is O2) or from fermentation (the acceptor is an organic molecule). Depending on their behavior towards O2, pathogenic bacteria can be classified as facultative anaerobic (use energy substrates through both the respiratory chain and fermentation), strict aerobic (multiply only in the presence of oxygen), strict anaerobic (die in the presence of oxygen) and aerotolerant anaerobic (Murray et al., 2009).
Bacteria causing infections in humans can be classified according to their taxonomic families and genus or according to the most relevant diagnostic features. The second classification is more interesting because it refers to clinically relevant characteristics, including Gram stain, shape, and respiratory tract (Table I).
V. ANTIBIOTHERAPY
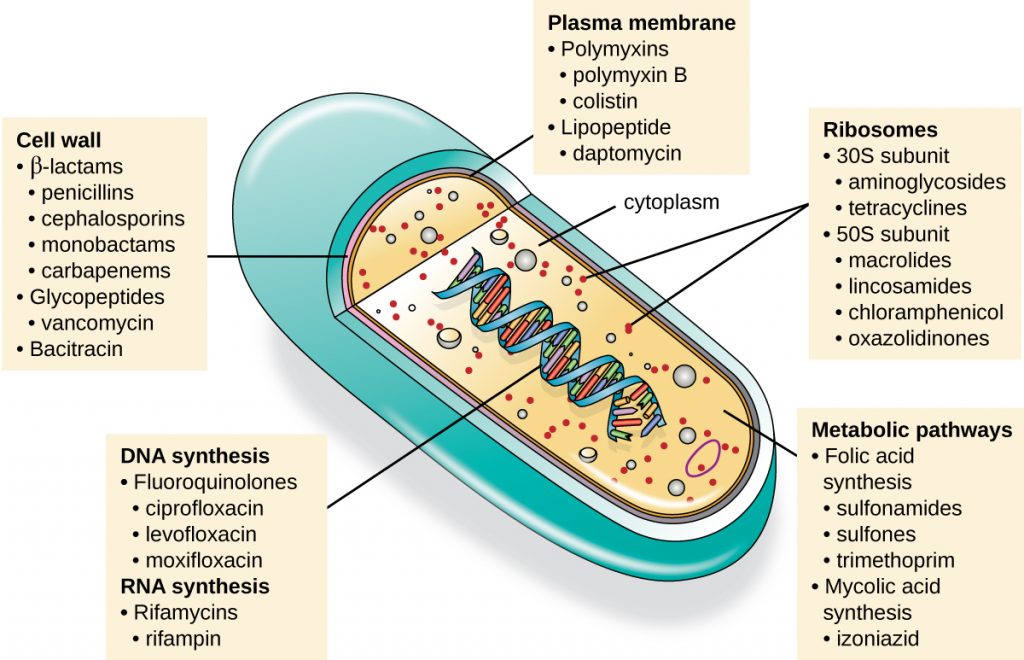
Antibiotics are natural, semi-synthetic or synthetic molecules that stop the growth of microorganisms or kill them. The antibiotics that stop the growth of microbes are bacteriostatic, those that kill microbes are bactericidal. In some circumstances, antibiotics can act as a bacteriostatic and in other conditions as a bactericide. They act by selectively blocking microbial processes on microbial cells. The main molecules used in antibiotic therapy have been natural products, developed by microbes under particular conditions to affect neighboring microbes, either to regulate their growth or to kill them (Walsh, 2003). Antibiotics are grouped into classes according to their targets in bacteria.
There are four main targets: bacterial wall synthesis, bacterial protein synthesis, bacterial DNA or RNA replication, and folate synthesis (Walsh, 2003) see Figure 1.
Table I Simplified Classification of Bacteria of Medical Interest (www.biotechnology-library.blogspot.com, MAJ 27 Feb2017)
| Aerobic bacterias | Gram + | Cocci | Staphylococcus, Streptococcus, S. Pneumoniae |
| Bacillus | Corynebacterium, Listeria, Bacillus | ||
| Gram – | Cocci | Neisseria, Mraxella | |
| Bacillus | E. Coli, Salmonella, Shigella, Klebsiella, Enterobacter, Serratia, Yersinia, Pseudomonas, Vibrio Campulobacter, Haemophilus, Brucella, Helicobacter | ||
| Intra-cellular bacterias | Rickettsia, Chlamydia trachomatis, C psitacci, Coxiella, Ehrlichia | ||
| Spiral Bacillus | Treponema, Borrelia, Leptospira | ||
| Bacteria without walls | Mycoplasma | ||
| Anaerobic bacterias | Veillon’s flora | Cocci and Bacillus | |
| Gram – | Bacillus | Bacteroides fragilis, fusobacterium | |
| Gram + | Bacillus | Clostridium tetani, C botulinum, C difficile, C perfringens | |
VI. ANTIBIOTIC RESISTANCE
The WHO has noted the occurrence of resistance to antibiotics, which is growing more and more, making it necessary to turn to other molecules for therapeutic purposes, particularly compounds of plant origin. Resistance to an antibiotic can be natural or innate (species whose wild strains are naturally resistant to certain antibiotics) or also acquired: when it appears in bacterial species that were previously sensitive to antibiotics. This resistance corresponds to an adaptation of bacteria to antibiotics (Rice et al., 2003).
It is therefore important to turn to traditional medicine in order to find new molecules to overcome these resistances.